Digest V25 N3 2015
http://www.omic.com/wp-content/uploads/2015/09/Digest-V25-N3-2015.pdf
Message from the Chair: Missed Diagnosis

I’m the daughter of an aviator.
I spent hours as a child sitting with my dad on the hood of a ’65 Mustang watching planes take off and land at Minneapolis/St. Paul International Airport. A former Air Force instructor pilot and Northwest Airlines captain, he taught me early on how 450 tons of aluminum can become airborne (Newton’s Third Law) and other aerodynamic concepts like pitch, yaw, attitude, and angle-of-attack. I still love talking to my father about airplanes and, like cable news outlets, often turn to my own resident aviation expert whenever a commercial airliner goes down. He is nearly always spot on when he predicts a crash was due to pilot error. Though each accident may have different antecedents, the final, often fatal mistake usually boils down to a simple failure of the flight crew to “fly the airplane.”
The 2009 crash of Air France 447, an overnight flight from Rio de Janeiro to Paris, is a classic case study in pilot error. Over the Atlantic, three hours into a routine flight, the crew started receiving faulty airspeed readings while entering a thunderstorm. Onboard computers, recognizing the erroneous airspeed was inconsistent with all the other normally functioning flight indicators, kicked off the autopilot. Forced to fly manually and distracted by the faulty airspeed, the crew (incorrectly) pulled the nose up, slowing the plane down and precipitating a stall. This error was further compounded when, in a departure from standard cockpit procedure, the pilots failed to monitor and call out loud the plane’s altimeter readings (how far up in the air the plane is). Recovering from a stall is as instinctive to an aviator as putting one’s hands out to break a fall: point the nose down, build up air speed, restore lift to the wing (Bernoulli’s Principle), and pull out into level flight. The crew had at least two minutes during their free fall to safely execute this maneuver but lost situational awareness of where they were in the air. Trying to troubleshoot the various alarms, confused and panicked by conflicting information, the pilots of Air France 447 literally forgot to “fly the airplane.” In under four harrowing minutes, the Airbus 330 dropped 38,000 feet from the nighttime sky killing all 228 aboard.
This issue of the Digest is dedicated to missed diagnoses, the medical equivalent of “forgetting to fly the airplane.” By one estimate, failure to diagnose kills over 40,000 people annually in American ICUs alone.1 That’s the equivalent of three Air France crashes every week. Plaintiffs alleged a failure to diagnose in 13% of OMIC’s 4,500 closed claims. It’s not the “zebras” we overlook; retinal detachment, glaucoma, and intraocular foreign bodies are among the top diagnoses we miss. The same factors contributing to pilot error—conflicting information, distraction, lack of communication, departure from preferred practice patterns—are at work in our clinical environments. Like those Air France pilots who failed to execute a successful recovery from their stall, we ophthalmologists usually have all the clinical information we need to make the correct diagnosis, even when we fail to do so. Maintaining situational awareness in high stakes, high stress situations—Why is this patient deteriorating? What could I be missing?—helps us to better connect the dots. Now sit back, relax, and read on for tips to keep you and your passengers, I mean patients, safe.
Rate decrease and policyholder dividend approved for 2016
OMIC’s Board of Directors is pleased to announce a nationwide rate decrease and a 20% policyholder dividend for insureds effective January 1, 2016.
After a favorable year buttressed by excellent claim results and lower than expected operating expenses, OMIC is experiencing one of our best years ever. In recognition of this development, we are implementing a rate decrease in all states totaling approximately $6 million nationally. The amount will vary by coverage area and insureds will be notified of the decrease in their territory.
Since 2005, OMIC has lowered rates by an average of nearly 40% nationally. OMIC continues to outperform competitors by making fewer and lower average indemnity payments than the multispecialty industry average.
OMIC will also apply a policyholder dividend for all physician insureds in the form of a 20% credit toward 2016 renewal premiums. Since the company’s inception, OMIC has announced dividend credits totaling more than $65 million, leading peer companies by a wide margin. Issuance of dividend credits is determined each year after careful analysis of operating performance. OMIC remains committed to returning premium above what is necessary to prudently operate the company and to do so at the earliest opportunity.
Issuance of the dividend requires that an active 2015 professional liability policy be renewed and maintained throughout the 2016 policy period. Mid-term cancellation would result in a pro-rata dividend. Dividends appear on your policy invoice as a credit to either your annual or quarterly billing installment. OMIC issues dividends as a credit toward renewal premiums for two reasons: premium credits offer favorable tax implications for policyholders and allow for easy and efficient distribution of dividends, which keeps operating expenses as low as possible.
2015 Claims Study: Giant cell arteritis claims are costly and difficult to defend
RONALD W. PELTON, MD, PhD, OMIC Committee Member, and ANNE M. MENKE, RN, PhD, OMIC Risk Manager
A 77-year-old male patient presented for the first time to our insured ophthalmologist to report the sudden onset of intermittent diplopia six days prior and a headache over his eyebrows for one day. Noting right inferior oblique muscle paresis but unable to determine its cause, and with no neuro-ophthalmologist in the region, the eye surgeon referred the patient to a neurologist. The patient told the neurologist that the headache had actually lasted for one month and that he was also experiencing jaw pain. This additional information prompted the neurologist to include giant cell arteritis (GCA, also known as temporal arteritis) in the differential diagnosis and to order an MRI, CT, and lab work.
When the patient saw the ophthalmologist about two weeks later, he reported a new symptom, a low-grade fever, with ongoing headache and diplopia. Five days after that—a full three weeks after the initial visit to the ophthalmologist—the patient lost vision in his left eye. An emergency room physician diagnosed giant cell arteritis and began intravenous steroid treatment, but the patient never regained vision in that eye. The malpractice lawsuit against the ophthalmologist settled for $85,000; we do not know the outcome of the suit against the neurologist.
Armed with hindsight bias, the classic signs and symptoms of giant cell arteritis jump out: older patient, vision changes, headache, jaw pain, and fever. It is hard to imagine how the definitive diagnosis and treatment were delayed for so long and easy to erroneously conclude that both physicians must have been incompetent. The claims investigation showed instead that these physicians had treated patients with giant cell arteritis, knew its signs and symptoms well, and understood that emergent treatment is needed to prevent imminent, bilateral vision loss. What, then, led these physicians astray?
Severe vision loss, costly claims
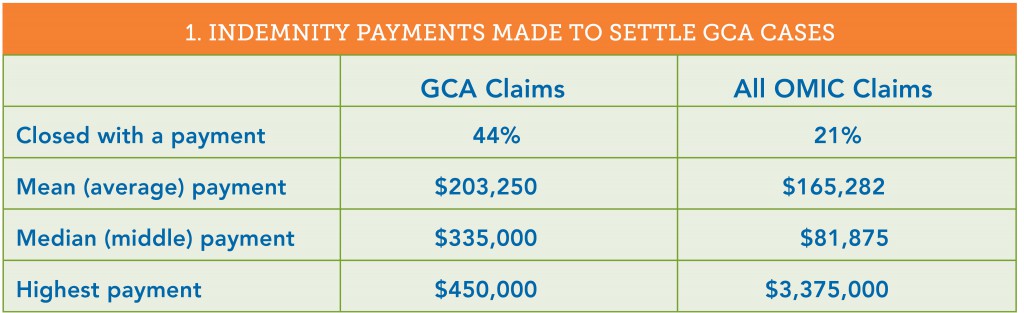
This issue of the Digest will report on a study of OMIC claims involving 18 patients diagnosed with GCA between 1993 and 2014. In 12 of the 18 cases (66%), no physician included GCA in the differential diagnosis. Four of these patients were seen only by an ophthalmologist; the rest were examined by an eye surgeon and one to three additional physicians. And although GCA was considered by the ophthalmologists in each of the remaining six cases, symptoms in five patients progressed when either the ophthalmologists or other physicians did not follow through to confirm the diagnosis and coordinate treatment. All 18 patients experienced severe vision loss, often bilaterally. OMIC had to settle twice as many of these claims as OMIC claims overall, and the mean and median payments were both considerably higher (see table 1).
The short window for diagnosis and treatment and the risk of severe bilateral vision loss make the high stakes of this relatively rare condition clear. This issue of the Digest will explore the reasons for these poor outcomes, the standard to which medical experts hold physicians who treat these patients, and the measures ophthalmologists can take to improve the likelihood of a correct and timely diagnosis.
Patients presenting with only visual problems
Giant cell arteritis, a systemic inflammation of the blood vessels that restricts blood flow causing organ and tissue damage, most commonly affects patients over the age of 50. In addition to the symptoms noted above and scalp tenderness, varied and non-specific constitutional symptoms, such as fatigue, malaise, and weight loss, may develop over time. It can be difficult to diagnose GCA when the only symptom is a change in vision. Four of the 18 patients presented this way. In two of these cases, defense experts supported the ophthalmologists’ care and the claims closed without payment, even though the insureds did not diagnose GCA or such diagnosis was delayed. In one case, a patient with dense cataracts that explained her vision loss was appropriately referred for work-up of a choroidal mass; the jury returned a defense verdict. In the second case that closed without a payment, a patient who presented with intermittent blurry vision was diagnosed with amaurosis fugax, a temporary loss of vision in one eye caused by a lack of blood flow to the retina. Because the patient was 79, the ophthalmologist ordered an erythrocyte sedimentation rate (ESR). When the result was normal at six, he repeated the test and got the same result. He diagnosed GCA six days later when the patient complained of a shade over the eye and developed a Marcus Gunn pupil and visual field deficit. OMIC declined the patient’s settlement demand and the case was ultimately dismissed. The two other cases where vision change was the only symptom were settled when OMIC could not find supportive defense experts. In one, the ophthalmologist noted papilledema in an 81-year-old who presented with sudden vision loss, but he did not work up its cause. The case settled for $275,000. In the other, the ophthalmologist was criticized for not clarifying the nature of the visual complaint. The 82-year-old patient had written on the history form that her vision “blacked out.” The surgeon did not read the form and documented only “blurry vision” and diagnosed her with visual migraine. The case settled for $350,000.
Problems eliciting a thorough and accurate history
Exploring the precise nature of the vision change would have helped another ophthalmologist entertain a GCA diagnosis. His patient complained of a headache for two days and a “curtain,” which he understood to be transparent. It was only during the investigation of the lawsuit that he learned the patient had experienced a “dark” curtain that caused frank vision loss. He felt, in retrospect, that the combination of vision loss and headache in an elderly patient should have alerted him to GCA and agreed to settle the claim for $100,000.
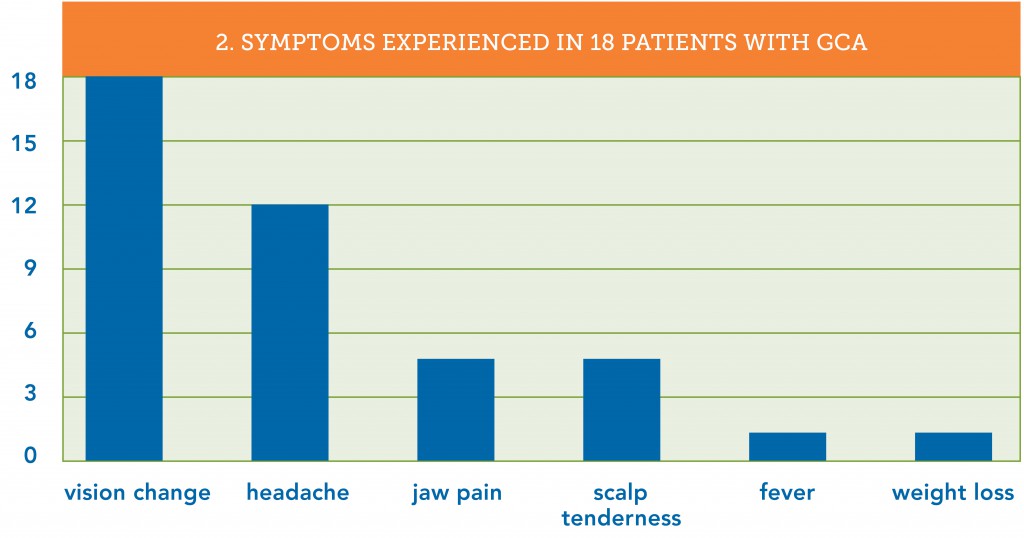
While it is important to get accurate information about the eye complaint, it is crucial to query older patients about constitutional symptoms. A careful review of signs, symptoms, and systems can help distinguish the few patients who could have GCA from the large number of older patients with eye problems seen daily in ophthalmic practices. Which symptoms did the patients in our study exhibit? Consistent with GCA’s usual appearance in patients over 50 years old, those in this study ranged from 62 to 86. As part of a claims investigation, defense attorneys obtain and review all of the patient’s medical records. These reviews revealed that 15 of the 18 patients (83%) were experiencing GCA symptoms other than vision changes at the time of their initial visit to the ophthalmologist. Of these 15 patients, 12 reported headaches and 7 of the 12 had additional symptoms (see table 2).
The ophthalmologists, however, failed to elicit the non-vision-related symptoms in 10 of the 15 patients (66%) who were having them. Defense experts opined that this inadequate history contributed to the delay in diagnosis and was below the standard of care. The ophthalmologist in the claim described in the beginning of this article learned only of the vision complaints and headache, while the neurologist, who saw the patient near the same time, elicited the duration of the headache and the existence of jaw pain. Ironically, the ophthalmologist testified in his deposition that he did not consider GCA in his differential diagnosis since the patient did not complain of jaw pain. He did not explain why he relied upon the patient to offer this information instead of asking for it.
Why is obtaining an accurate history so difficult? First, patients often report their history differently to each healthcare provider based upon the questions asked and the time spent gathering the information. Often it was other physicians who obtained a more thorough history, but in two of our claims, the ophthalmologists’ staff members obtained and documented the presence of GCA symptoms. Not only did the ophthalmologists not get the same information when questioning the patients a few minutes later, they also did not review the notes made by their staff members. This lapse was criticized by defense experts and contributed to the decision to settle these claims. Second, patients presenting with eye complaints often do not think that it is important or pertinent to tell their ophthalmologist about non-ophthalmic problems they are experiencing. More than in most diseases, however, prompt diagnosis of GCA depends upon the thoroughness and accuracy of the health history. In each of the 15 claims where patients had more than just visual symptoms, the plaintiff expert alleged that the diagnosis could have been made earlier if the ophthalmologist had obtained a more thorough history. Ophthalmologists examining older patients, especially those with vision changes and headache, need to take a more active role in obtaining the history. Dr. Ron Pelton, a practicing oculofacial surgeon who serves on OMIC’s claims and underwriting committees, has developed a GCA checklist to prompt ophthalmologists to ask key questions and document both positive and negative findings. It can be found at Giant Cell Arteritis Checklist.
Missed opportunities
So what happened in the first case? While the ophthalmologist did not elicit a thorough history or include GCA in his differential diagnosis, the neurologist to whom he referred the patient did ask the appropriate questions. The combination of diplopia and pain in the temporal mandibular joint led the neurologist to a robust differential diagnosis, which included right fourth nerve palsy versus right inferior oblique paresis, brain stem ischemia, myasthenia gravis, and vasculitis. He appropriately ordered an MRI, CT scan, and laboratory work, including an ESR. About a week after he examined the patient, the neurologist realized that the lab had mistakenly not performed the ESR. He mailed the patient a prescription to have it done the next day but the patient never went. Six days later, the patient brought the results of the MRI, CT, and lab work (minus any ESR results) to his second visit with the ophthalmologist, who skimmed the report, which discussed the non-specific MRI and CT results and the normal lab results. He failed to notice that the lab had not performed the ESR. While he did see that the patient had been given a prescription to have the ESR repeated six days prior, he assumed the test had been done and was again normal. The ophthalmologist advised the patient to keep his follow-up appointment with the neurologist in four days time. Experts who reviewed the claim felt that four opportunities for an earlier diagnosis that would have preserved the vision had been lost: when the lab did not perform the first ESR ordered, when the patient did not go back to get the ESR lab test done, when the neurologist did not follow up to ensure it was done, and when the ophthalmologist failed to note the lack of ESR results. Had the ophthalmologist asked the patient, he would have learned that no ESR had been done. This information, combined with the new symptom of fever, could have prompted him to consider GCA and order a stat ESR.
Preventing vision loss
This constellation of incomplete history, poor coordination of care among physicians, and problems with patient adherence occurred in many of the claims, including the one in the Closed Claim Study. This article provides information on actions ophthalmologists can take, such as proactively obtaining a more thorough history, to improve the likelihood of including GCA in the differential diagnosis when older patients present with vision changes. The checklist created by Dr. Pelton can prompt such questions and help track the completion of key tests and consults. A robust appointment and test tracking system plays a pivotal role in preventing diagnostic error (see “Test Management System is Key to Prompt Diagnosis” and “Noncompliance” at www.omic.com for advice on how to implement one). The Hotline article in this issue provides recommendations on ways to improve communication with other physicians and your staff.
2015 Claims Study: Clear communication is key to timely diagnosis and treatment
ANNE M. MENKE, RN, PhD, OMIC Risk Manager
The claims discussed in the lead and Closed Claim articles resulted partly from poor communication among treating physicians and staff members. Here are some recommendations about ways to ensure that the necessary information is received from and communicated to the appropriate members of the healthcare team. The scenarios come from actual giant cell arteritis (GCA) claims, and some of the “advice” is from the defense experts who reviewed the claims.
Q An emergency room physician from one of the local hospitals called me about a patient of mine. I don’t take call at that hospital and told him to have the patient schedule an appointment with me. Now I’m being sued along with the ER physician, who says he informed me that the 72-year-old patient had a headache and vision loss. The lawsuit says I should have at least warned the ER physician about GCA. What was I required to do?
A You have no legal duty to provide assistance to a hospital when you are not on call for it. As an ophthalmologist, however, you know more about the risk of severe vision loss from GCA than an ER physician. To protect the patient, urge the ER physician to contact the on-call ophthalmologist to evaluate the patient. (The claim closed without a payment.)
Q I work in a practice that employs optometrists. One of them asked for my opinion about a 67-year-old patient who presented with vision loss, a headache, jaw pain, and scalp tenderness. The OD thought the patient had GCA. I agreed and told him to start steroids and provided the starting and maintenance dosages. The technician who was scribing made a mistake and wrote the prescription for 20 mg daily instead of four 20 mg tablets daily. Now I’m being sued for not taking over care of the patient from the OD and not adequately supervising the technician. What should I have done?
A Optometrists often perform the initial evaluation for patients in a group practice. However, when a patient has a serious, vision-threatening condition such as GCA that requires urgent treatment and careful coordination of care, an ophthalmologist should assume responsibility. Your practice’s written protocols should address this (see “Coordination of Care with Optometrists” at www.omic.com). This optometrist did not have the legal authority to prescribe systemic steroids. In addition, while your technician may know the names and dosages of the eye drops you normally prescribe, she is obviously not familiar with oral steroids. You should have written the prescription yourself and provided written instructions to the patient on how much to take each day and when to see her primary care physician (PCP). Finally, you should have conducted a formal hand-off with the PCP to clarify that the PCP would be responsible for ongoing management of the steroids. It is helpful to give the patient a referral note that explains the reason for the referral and when it should take place (available at www.omic.com/referral-note-for-patient/). (The claim settled for $350,000.)
Q A 76-year-old patient called our practice and spoke to my technician, who reported the conversation to me. I recall her telling me that the patient had pain in the back of his neck, so I instructed her to tell him to see his PCP. The lawsuit alleges that we were told that the pain was also in the temple area and accompanied by visual disturbances, and that given his age, I should have seen him right away. Am I expected to speak to each patient myself or review each note about phone calls?
A You obviously cannot talk to every patient who calls, so you need an efficient and effective way to share information. OMIC claims experience makes it clear that making medical decisions on the basis of the limited information obtained over the telephone is a risky, albeit necessary, aspect of ophthalmic practice. During the phone call, you and your staff need to gather the information necessary to assess the situation and determine the treatment plan, communicate the assessment and plan to the patient, and document the encounter and your decision-making process in the medical record. To ensure that you have the most accurate information, provide staff with a checklist of questions to ask and instruct them to document the answers. Review the contact form when you can give it adequate attention, and document the information you would like your staff to communicate to the patient. To assist you, OMIC developed a sample phone contact checklist and appointment scheduling guide called “Telephone Screening of Ophthalmic Problems” available at www.omic.com. Use this guide to develop written protocols for telephone screening and treatment that are specific to your patient population, subspecialty, and staff; train staff in the use of the protocols and verify competency; and willingly accept questions from staff members unsure of how to handle specific calls. (This claim settled for $200,000.)