
Risk Management
| << Back | Download |
When patients fall, are doctors to blame?
ANNE M. MENKE, RN, PhD, OMIC Risk Manager
Mrs. B, a 73-year-old woman with a number of medical conditions, came to her ophthalmologist’s office for an eye exam. She was asked to sit on a stool with wheels for the exam. She slipped off, landing on her tailbone. X-rays revealed a possible hairline fracture of the spine. When Mrs. B suffered bruising and ongoing pain, she filed a claim against the ophthalmologist. She never regained the ability to walk and died nine months later. Her claim settled for $60,000.
Falls are the leading cause of fatal and non-fatal injuries for people over 65 years of age, according to the Centers for Disease Control (CDC). They stem from intrinsic factors related to the individual, such as age, health problems, and medications. Or they can result from extrinsic, environmental circumstances, such as wet floors or poor lighting. A fall compounds the burden of preexisting health problems and can precipitate an inexorable decline. Indeed, 20% of older people who fall die within one year of the mishap, like the patient discussed above. Many of these falls occur in the home. When they happen in physician offices and ambulatory surgery centers (ASCs), some patients and their families assume that physicians and staff members should have predicted and prevented the fall, and they sue for malpractice.
OMIC has handled 50 claims and lawsuits involving 41 patients who have been injured during falls, about 1% of our total claims since 1987. Of these 50 claims, 46 are now closed. The 41 patients who filed these claims are similar to those studied by the CDC: all but ten were over age 60, and four died, three within the first year after the accident. Forty patients sustained significant injuries and faced unexpected medical costs. Twenty-five had fractures, including of the skull, nose, arms, ribs, spine, hip, legs, and feet. The remaining patients had rotator cuff tears or serious soft tissue injuries to the head, hip, and upper and lower extremities. But were the falls due to negligent care? Could they have been prevented? This issue of the Digest will examine the circumstances surrounding falls, determine factors that increase their likelihood, and offer suggestions on ways to identify and assist those most at risk.
When is a fall the result of negligent care?
When patients who fall sue their ophthalmologists, they usually allege that the fall should have been prevented by maintaining a safer environment, better assisting the patient, or both. Therefore, most investigations of fall claims will include not only an analysis of the patient’s medical condition and the care provided by the ophthalmologist and staff, but also a review of the environment.
Such an investigation was conducted after a 79-year-old woman who presented for a dilated eye exam fell and sued her ophthalmologist. As they had done after all of her prior dilated exams, the ophthalmologist’s staff members offered her sunglasses as she was leaving the office to help reduce her light sensitivity. She declined the offer. After she exited the darker office into the sunlight, she lost her balance on a set of stairs and fell down, breaking her hip. An analysis of the incident showed that the patient was healthy and the care of the ophthalmologist’s staff was appropriate. The attorney defending the physician then conducted an inspection of the premises. He noted that the first step was about eight feet from the door. There were handrails on both sides and down the middle of the stairs. Each step was three feet long, with the edge painted black. He felt that the steps were constructed as safely as possible and were in good condition. He concluded that even if the patient was temporarily “blinded” by the bright sunlight as she claimed, she nevertheless had space and time to allow her eyes to adjust before starting down the stairs. The attorney filed a motion for a summary defense judgment as no expert had alleged that the eye physician or his staff had been negligent, perhaps because this was a healthy patient who knew what to expect after dilation and declined the offer of sunglasses. The motion was granted, and the case was dismissed.
In fall-related lawsuits, plaintiffs may allege professional liability (PL or medical malpractice) or general negligence (GL or premises liability). Professional liability is negligence based on a breach of the standard of care in the performance of healthcare services. Premises liability occurs when a business owner does not adequately protect its patrons from hazards on the premises. Therefore, in order to determine whether a case is really a PL or GL claim, courts will often look at whether the patient was actually receiving medical care at the time of injury. They may also look at whether the service being provided requires special knowledge, licensing, or accreditation. This distinction is important for a variety of reasons that are explained in the Policy Issues article.
Payments for falls
The decision to settle a claim is usually based upon reviews provided by OMIC’s consultants or experts hired by the defense attorney, and after consultation with and consent from the insured ophthalmologist or ASC. However, it is not always necessary to obtain expert opinions for claims when patients fall, as the injuries are evident and the allegations and investigations relatively straightforward. OMIC settled 18 of the 46 closed claims (39% of them) related to falls. This percentage is almost twice as high as for our claims experience overall (see table 1). There are several reasons for this. 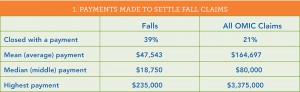
First, ophthalmologists, their practices, and ophthalmic ambulatory surgery centers often quickly elected to settle claims involving severe injuries, obviously frail patients, or those using assistive devices, such as canes, walkers, or wheelchairs.
Second, while physicians were often named as defendants in these claims, the falls generally occurred while the patient was with staff. Accordingly, settlements were made on behalf of the practice or ASC and the physician was dismissed from the claim. Such a resolution has an added benefit: while indemnity payments made on behalf of physicians and other licensed healthcare practitioners must be reported to the National Practitioner Data Bank, no such report is required for entities.
Finally, the mean and median payments were significantly less than for OMIC’s total claims, as was the largest payment. The highest payment for a fall occurred after an 82-year-old woman fell when asked to move onto a chair with wheels. When the chair went out from under her, she fractured her hip. She required surgery, an extensive hospitalization, and care in a nursing home, leading to $100,000 in medical expenses. When Medicare learned how the fracture occurred, it refused to pay for her care. OMIC settled the claim for $235,000. (OMIC’s highest-ever indemnity payment of $3,375,000 was for failure to diagnose retinopathy of prematurity.)
When and where do eye patients fall?
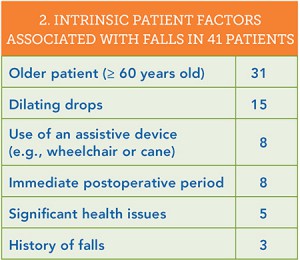 In an attempt to learn what can lead to falls, we analyzed both the patient characteristics associated with the falls and the actions that immediately preceded them (see tables 2 and 3). Thirty of the 41 patients fell during or just after office visits; the remaining 11 fell at an ambulator
In an attempt to learn what can lead to falls, we analyzed both the patient characteristics associated with the falls and the actions that immediately preceded them (see tables 2 and 3). Thirty of the 41 patients fell during or just after office visits; the remaining 11 fell at an ambulator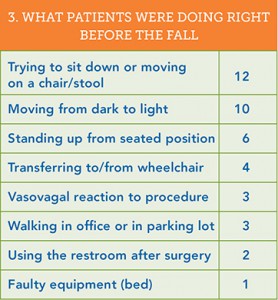 y surgery center. After the patient’s age, the most common intrinsic factor associated with a fall was the use of dilating drops: fully half of the patients who fell at the office did so after a dilated eye exam. Dilating drops are an essential aid to diagnosis. Yet they are known to cause temporary vision problems, such as light sensitivity, glare, and decreased contrast sensitivity. These drops may be more apt to pose problems for older patients since it can take longer for their eyes to judge distance and depth and to adjust to sudden changes from dark to light. Indeed, 10 patients fell when moving from the darker interior of the office into the brighter outdoors, including patients wearing sunglasses or transitional lenses.
y surgery center. After the patient’s age, the most common intrinsic factor associated with a fall was the use of dilating drops: fully half of the patients who fell at the office did so after a dilated eye exam. Dilating drops are an essential aid to diagnosis. Yet they are known to cause temporary vision problems, such as light sensitivity, glare, and decreased contrast sensitivity. These drops may be more apt to pose problems for older patients since it can take longer for their eyes to judge distance and depth and to adjust to sudden changes from dark to light. Indeed, 10 patients fell when moving from the darker interior of the office into the brighter outdoors, including patients wearing sunglasses or transitional lenses.
The most frequent action leading to a fall was moving onto a chair or stool or changing position while on one. Experts who reviewed claims involving falls from stools or chairs with wheels criticized their use, especially in elderly patients who were left unattended. Standing up from a seated position precipitated six falls. Older patients may experience drops in blood pressure when standing up and thus feel faint. This is even more likely right after surgery involving sedation or anesthesia: eight patients fell in the immediate postoperative period. Older patients often do not have strong muscles in their abdomen or legs and need to use their hands to push off from chairs to stand up. Younger ones who fell when getting up had vasovagal episodes after injection of fluorescein or minor eye procedures. Eight patients fell who used mobility aids, such as canes, walkers, and crutches, including four patients who fell while moving into or out of their wheelchairs.
What assistance should be offered to patients?
This review of 41 falls offers some guidance on which patients are likely to fall, and the Hotline article provides additional screening tools. By asking some simple questions and watching for certain behaviors, ophthalmologists and the eye care team can identify those most at risk. The next step in fall prevention is to provide assistance. But which patients should be helped? Are staff in offices expected to escort each patient whose eyes have been dilated to the front desk? Should they and staff at ASCs take all patients to their cars? Eye practices and ASCs clearly do not have the personnel to provide this level of individual assistance. And while plaintiff attorneys have alleged that this help was required and should have been provided, experts hired by defense attorneys to evaluate fall claims did not agree. They made it clear that staff should not be expected to assist patients who function normally outside the office, even if their eyes are dilated. They were critical, however, when the physician and staff did not provide monitoring and assistance for patients who had obvious difficulty ambulating and moving.
Back in 1992, OMIC Board member Dr. Monica L. Monica offered some “common sense safety tips” to minimize the likelihood of a general liability claim (http://www.omic.com/making-your-office-safe/). Her suggestions on which patients to assist are still pertinent today. Please see her article for more detailed advice on making the office environment safe.
- Watch and assist patients when seating them on stools. Make sure the rollers of the stool do not easily slide, carrying the stool out from under the patient. Stools with locking devices are preferable, especially when performing office laser procedures.
- Supervise and assist patients with mobility problems at all times when being moved in and out of exam rooms or on and off chairs. This is especially important for individuals who are blind or have low vision.
- Stay with elderly patients in exam or treatment rooms.
- Encourage patients whose pupils have been dilated to stay in the office until they are comfortable with their vision. Provide post-mydriatic spectacles or drops to reverse dilation. Suggest that patients take a taxi home or arrange for a family member or friend to drive them.
Falls cause significant injury. Ophthalmologists and the entire eye care team can help prevent them. To assist in staff education, key information in this issue of the Digest has been summarized in “Fall Prevention,” available at http://www.omic.com/fall-prevention/.
Please refer to OMIC's Copyright and Disclaimer regarding the contents on this website







